Patient Eligibility
Infinedi partners with multiple top industry leaders to provide all-payer eligibility verification. Your staff can effectively assign and prioritize patients, manage payer related tasks, and create individualized payer-specific notes to help your staff manage multiple activities.
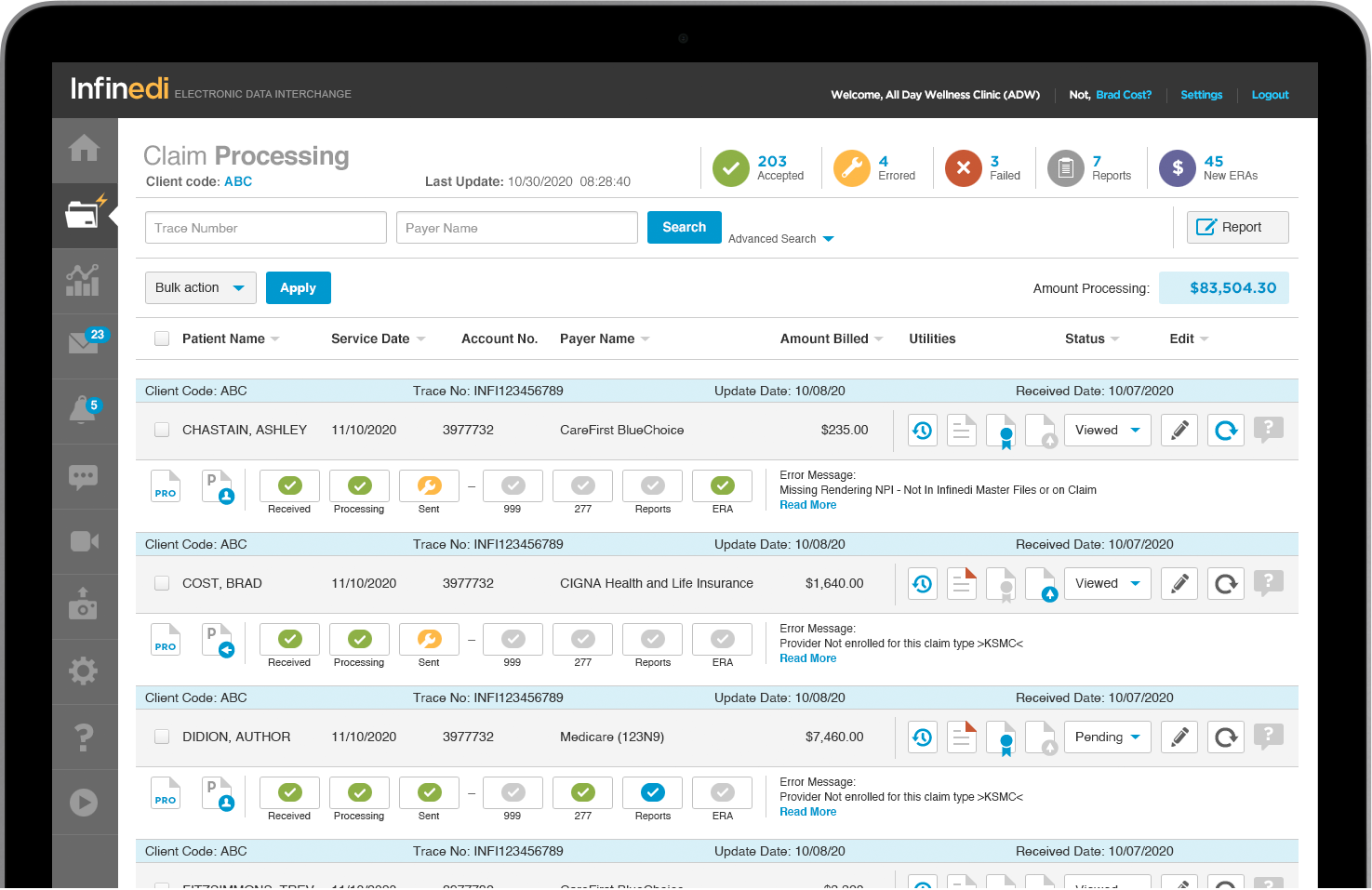
Using these powerful customizable dashboard, you can create customized task filters to ensure that accounts receive proper follow-up and resolution.
These filters allow supervisors to assign tasks to areas of billing, admission or reimbursement within a single location or multiple facilities.
The dashboard filters benefit information, and additionally sends alerts if there is a detected coverage overlap. This system also has a batch function in which you can enter multiple patients and check multiple payers in one simple step.
Request a personalized demo
Your personalized demo will include an overview of our fast and easy to use Infinedi claims processing stoplight graphic system. Plus, we'll take a look at Infinedi Analytics – the software that provides your team with the tools and insight it needs to make data-driven-decisions that grow business and keep you ahead of the competition.